A Step-by-Step Guide to Short-Term & Long-Term Disability Insurance Benefits for Mental Health Conditions
While most people think of disabilities as physical and observable conditions, not all disabilities are outwardly apparent. In fact, mental health conditions are among the top causes of disabilities in Wisconsin and across the United States. Some of the most commonly debilitating mental health conditions include depression, anxiety, PTSD, OCD, eating disorders, and substance use disorders. However, unlike physical disabilities, these mental health conditions can’t be diagnosed with an x-ray, MRI, or physical assessment. Instead, medical providers must rely on patients’ reported symptoms and observations of their demeanor to diagnose a condition.
Mental health conditions can be as debilitating as any physical injury or illness. As such, individuals living with mental health conditions may experience periods of time when their condition significantly interferes with their ability to work. Since financial stress exacerbates mental health conditions, having a continued source of reliable income is an important tool for recovery.
In addition to federal programs run by the Social Security Administration, individuals struggling with a debilitating mental health condition may qualify for additional benefits under their employer-sponsored short-term or long-term disability insurance (STDI or LTDI) policies. However, the subjective nature of mental health conditions makes it difficult for individuals to “prove” their disabilities for purposes of obtaining these benefits.
This article explains:
• the application filing process for STDI/LTDI benefits,
• what to do if your application is denied, and
• important considerations for claimants disabled by mental health conditions.
Filing a Claim for STDI/LTDI Benefits
Who is Eligible to Claim Disability Benefits?
If your employer offered STDI or LTDI coverage and you enrolled in this coverage (not every employee does), you are eligible for these disability benefits. Typically, you must have been covered under the policy for a specific amount of time before you are able to file a claim for benefits. Your policy’s Summary Plan Description and/or Plan Document will explain this specific time period.
You should have automatically received a copy of the Summary Plan Description when you enrolled in coverage. While you do not automatically receive a copy of the Plan Document, you may request a copy from your “plan administrator” (generally, the plan administrator is your employer).
How Do I File a Disability Benefits Claim?
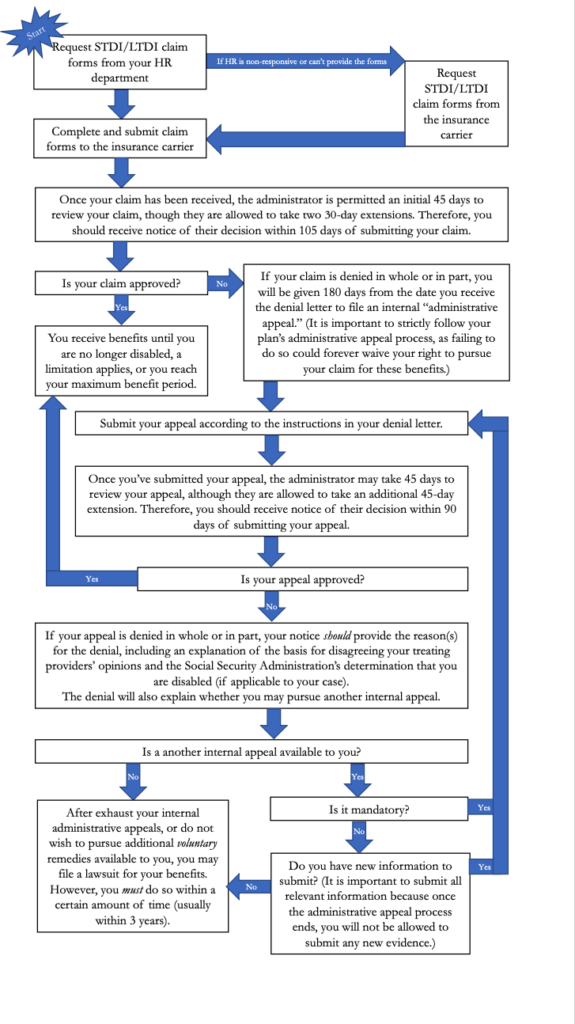
To start your disability benefits claim, you should request STDI/LTDI claim forms from your plan administrator, which is probably your HR department. If you are unable to get these forms from the HR department, you can reach out directly to the “claims administrator” (generally, the claims administrator is the insurance company that insures the policies). The claims administrator and their contact information should be listed in your policy documents.
Application Documents Required from You, Your Employer, & Your Doctor
In most cases, the claim forms are comprised of three parts:
(1) a form for you to complete, sometimes referred to as the “Claimant Statement” or “Employee Statement,”
(2) a form for your employer to complete, sometime referred to as the “Employer Statemen,t” and
(3) a form for your treating provider to complete, sometimes referred to as the “Attending Physician Statement.”
The Claimant/Employee Statement may ask about your educational and employment history and how your condition impacts your daily life. The Employer Statement asks for information about your rate of pay and job duties.
Your Doctor(s) Opinion is Critical to a Successful Claim
Finally, the Attending Physician Statement asks about the ways your medical condition impacts your ability to function. For that reason, it is exceedingly important to be seeing a doctor who agrees with your need to take a medical leave from work in order to have a successful claim for these benefits.
Additionally, if you see more than one doctor/provider for your disabling mental health condition, you should ask each one to complete a form. For example, you may be under the care of both a therapist and a psychiatrist to treat your mental health condition. In this case, you should have both the therapist and the psychiatrist complete the Attending Physician Statement.
Disability Claim Filing Deadlines
Generally, completed disability claim forms should be submitted directly to the claims administrator. However, you should review your claim forms for specific instructions for submission. Once your claim has been received, the claims administrator is permitted an initial 45 days to review your claim, though they are allowed to take two 30-day extensions. Therefore, you should receive written notice of their decision within 105 days (3 ½ months) of submitting your claim.
How Long Can STDI and LTDI Benefits Last?
Each policy is different so be sure to consult your Summary Plan Description and Plan Document. STDI benefits typically last anywhere from a few weeks to a year or more. Once you have exhausted your STDI benefits, you may transition to LTDI benefits if you are eligible. In this case, you should request the LTDI claim forms in advance of the date your STDI benefits end to avoid delay in the processing of your LTDI claim.
For most long-term disability policies, LTDI benefits continue until you reach age 65 or your social security normal retirement age, assuming you remain disabled. However, certain limitations may apply. For example, LTDI policies are allowed to distinguish between claims based on mental health conditions and physical conditions. Accordingly, many LTDI policies include a “Mental Illness Limitation,” which limits the payment of LTDI benefits to 24 months for disabilities based on a mental health condition or substance use disorder.
Mental Health Conditions Resulting from Physical Injuries
If your mental health condition developed as a result of a physical disability, your claim should not be subject to the Mental Illness Limitation. For example, Joe suffered a serious car accident resulting in disabling chronic back and neck pain. As a result of this pain, Joe could no longer participate in his favorite activities, such as fishing and hiking. Likewise, he could no longer travel long distances to visit friends and family. These changes, coupled with his ever-present pain, caused Joe to develop loss of interest, feelings of hopelessness, and low self-esteem. Later, Joe was diagnosed with depression. Even though Joe’s depression may be debilitating, because it resulted from his chronic back and neck pain, his claim for LTDI benefits should not be subject to his policy’s Mental Illness Limitation.
To discern whether a mental health limitation applies to your claim for LTDI benefits, see our specific article on this question.
What to Do If Your STDI/LTDI Benefits Claim Is Denied
How Do I Know if my Disability Claim is Denied?
If your claim is denied in whole or in part, you will receive written notice of the denial. This “denial letter” will include:
• the specific reason(s) for the denial
• reference to the policy provisions upon which the denial is based
• a description of any additional information that may be necessary for you to perfect your claim, including why such information is necessary
• a description of the policy’s internal administrative appeal procedures
• an explanation of the claims administrator’s basis for agreeing or disagreeing with your treating providers’ opinions, the medical experts it hired to review your claim, and the Social Security Administration’s determination you are disabled (if applicable).
How do I File a Disability Claim Appeal?
You have 180 days from the date you receive the disability claim denial letter to file an internal “administrative appeal.” The denial letter will include instructions for submitting the appeal. It is important to strictly follow your plan’s administrative appeal process, as failing to do so could forever waive your right to pursue your claim for these benefits.
What Should I Include in the Disability Claim Appeal?
In addition to including the information described in the denial letter as being necessary to perfect your claim, you may also consider including the following:
• Updated medical records.
• A letter from your treating providers regarding the ways in which your medical condition impacts your ability to function.
• A personal statement from you explaining the ways in which your medical condition has impacted your daily life.
• A letter from close friends and family members describing what they have witnessed in terms of your ability to function.
• A list of any medications you are taking to treat your condition, including a statement identifying any adverse side effects from medications.
• If your claim is based on a mental health condition, you may want to ask your treating provider to refer you for a psychological evaluation. Such evaluations are considered compelling evidence of your disability because they use standardized testing and assessment tools to arrive at a diagnosis and treatment plan.
It is important to include as much supportive information with your disability claim appeal as possible. Once you have exhausted your LTDI policy’s internal administrative remedies, your claim file is closed and you are unable to add additional evidence at a later date.
Additionally, claims administrators may try to deny benefits on the basis that a claimant has not provided “objective medical evidence” of their mental health condition. If this happens to you, your denial letter should also explain that it is unfair and unreasonable to require you to prove your mental health condition with objective data in light of the fact that no definitive objective test exists for the condition or its severity.
What Happens While the Appeal is Being Reviewed?
Once you’ve submitted your appeal, the disability claims administrator is allowed an initial 45 days to review your appeal, although they are permitted to take an additional 45-day extension. During this time, the claims administrator may contact you with questions related to your claim or request additional information from you. To avoid delay, it is important that you respond to such inquiries immediately.
The claims administrator may also refer your file for an independent medical review. This means a hired doctor will review your medical records and offer an opinion as to whether your conditions necessitate any restrictions/limitations. For mental health conditions, the independent medical reviewer will pay attention to your treatment’s frequency and intensity, whether your doctors increase or adjust your medications, and whether your daily activities correlate with your reported symptoms.
Additionally, in some cases, the claims administrators may even have you surveilled.
Before the claims administrator can render a decision on your appeal, they must provide you with an opportunity to respond to “any new or additional evidence considered, relied upon, or generated by the plan, insurer, or other person making the benefit determination in connection with the claim.” For example, if the claim administrator obtained an independent medical review or surveillance evidence, they must provide a copy of that review or evidence to you and allow you a reasonable amount of time to respond. Though your response is not mandatory, it does offer you another opportunity to explain why you meet your policy’s definition of disability.
What Should I do If My Appeal is Denied?
If the claims administrator decides to uphold their decision to deny your claim, their “uphold letter” will contain information similar to that of the initial denial letter. Importantly, the uphold letter will explain whether you have any other administrative remedies available to you, such as a second-level appeal.
If you have the option to pursue a second-level appeal, you may wish to take advantage of it because it provides you another opportunity to submit additional evidence in support of your claim. (As a reminder, once you have exhausted the administrative appeal process, you will not be able to submit any additional evidence.) For example, you may submit updated treatment records or ask your treating provider to write a letter rebutting the conclusions of the claims administrator’s hired doctor.
If you do not have the option to submit a second-level appeal, your next step is to file a lawsuit in federal court. If you have not already done so, it is imperative you speak with an attorney at this point.
Be Prepared to Seek Legal Help
If you are struggling to navigate the STDI/LTDI application or appeal process, contact a STDI/LTDI attorney at Hawks Quindel. Contingent representation may be available if you cannot otherwise afford an attorney.
Remember, if you or a loved one are struggling with a debilitating mental health condition or substance use disorder, there are resources available to you. Though it can be difficult to reach out, it is important to take that first step so you can connect with the support you deserve.

